CHAPTER 3 Reference Readings
Lesson 12
How do antibiotics work?
Designed to kill (but not us!)
It’s easy to kill bacteria on surfaces with things like bleach or hand sanitizer. But once they’re inside our bodies, we need to kill them with something that won’t be harmful to our own cells and bodies. To do this, antibiotics need to target structures that are specific to bacterial cells—structures that human cells do not share.
Bacterial cells and human cells have important differences
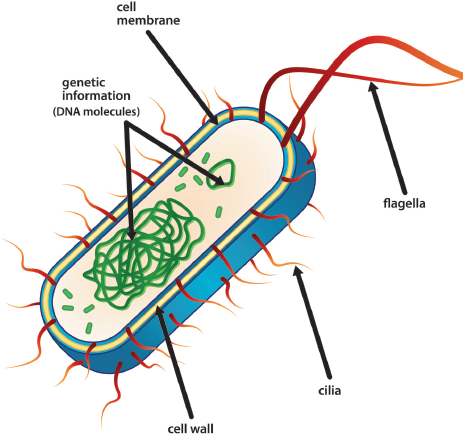
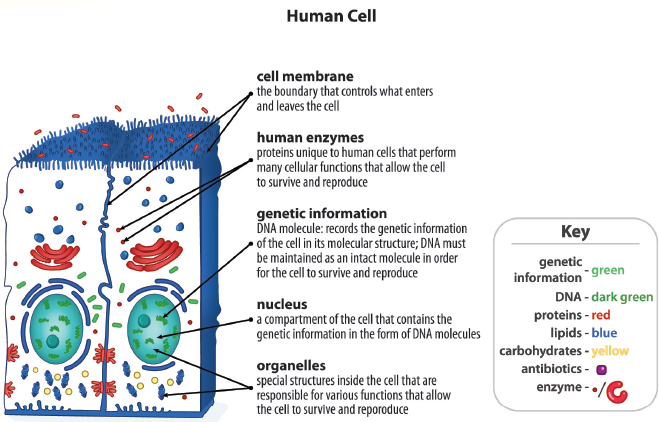
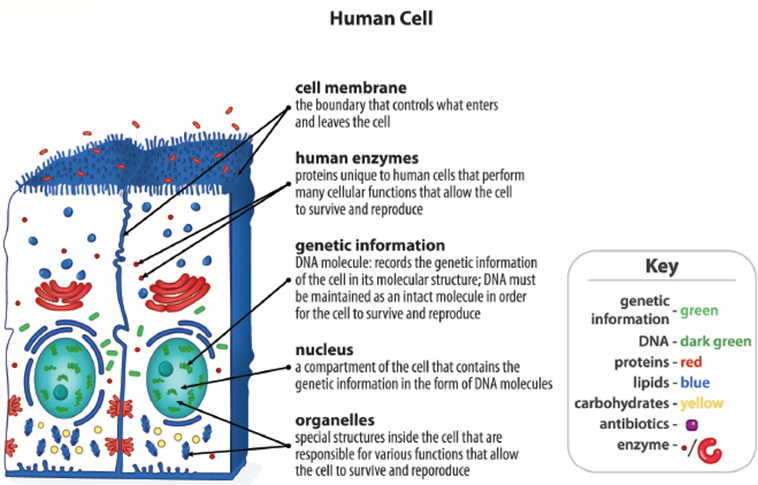
“Bacteria” refers to a large group of single-celled organisms. Both bacterial cells and human cells have DNA as their genetic material. Cells from both groups are surrounded by a cell membrane. Bacteria have cell walls in addition to cell membranes, while animal cells do not have cell walls.
Despite their similarities, bacteria and human cells have important differences. The biggest difference is that bacteria have cell walls, while human cells do not. Human cells have internal compartments enclosed in membranes. Bacterial cells also have different enzymes (a type of protein molecule) from human cells.
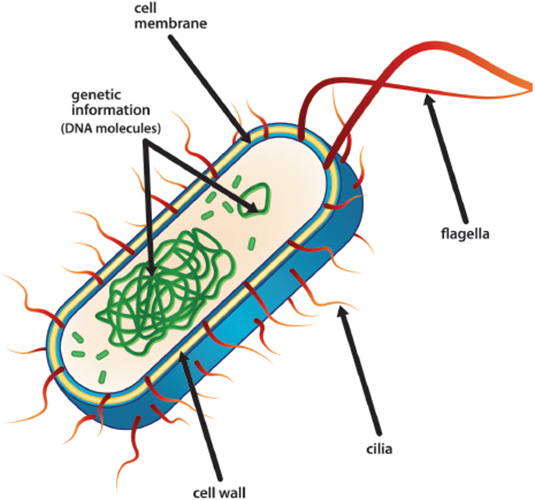
Bacteria and human cells. a. The bacterial cell shows a cell wall in addition to the cell membrane. b. The human cell shows distinct membrane-bound cell organelles. The large, roundish structure in the center is the nucleus.
A brief history
Before antibiotics were available, bacterial infections killed many people. Researchers discovered a few antibiotics in the 1920s, but they were not widely available until the 1940s. They quickly became important tools for fighting bacterial infections. Today, medical professionals choose from a wide variety of antibiotics to treat infections such as strep throat, pneumonia, and acne. But not every antibiotic is effective against all bacteria. Doctors must know which bacteria are causing the illness so they can prescribe an antibiotic that can kill that particular bacteria.
Mechanisms
Examples of antibiotics include penicillin, amoxicillin, ciprofloxacin, and vancomycin. Some of these medicines work by preventing bacteria from making cell walls. Bacterial cell walls are needed to keep the cells from bursting open and dying. Antibiotics that prevent cell wall formation work by killing bacteria. They do not harm human cells, because our cells do not have cell walls. Other antibiotics work by interfering with enzymes that affect protein synthesis. If bacteria cannot make the proteins they need, they stop growing. These antibiotics are effective because they prevent bacteria from growing and reproducing. They have little effect on human cells, because they do not interfere with the way our human enzymes function.
It is important to know that antibiotics are not effective treatments for infections caused by viruses. Viruses infect and “take over” an organism’s cells. They do not have cell walls, and they use enzymes from the organism’s cells to reproduce themselves. Thus, antibiotics that work by interfering with bacterial cell wall formation or enzymes have no effect on the growth of viruses.
Antibiotics don’t always kill all infecting bacteria
Even when antibiotics are used and taken correctly, they may not kill all of the problem bacteria. Even in a laboratory setting, each individual bacterium may, by chance, not encounter sufficient antibiotic molecules to result in killing it. These interactions are probabilistic, rather than certain.
Antibiotics are designed to work alongside the human immune system. By greatly reducing the number of bacteria, the immune system can often take care of the rest. If not, however, the remaining bacteria will begin growing and reproducing again and the population will increase. In these cases, the infected person may need a higher dose of the antibiotic, or another antibiotic may need to be tried.
You may wonder why medical professionals don’t use higher doses or different antibiotics in the first place if they know that at lower doses, some bacteria are likely to keep growing. The answer is that even though antibiotics are relatively safe medicines, they do have side effects.
Antibiotics are “wonder drugs” because they kill bacteria without harming our own cells. However, in higher doses, some antibiotics have more serious side effects. Vancomycin is often used as an antibiotic “of last resort” because it has serious side effects, such as the possibility of hearing loss and kidney damage.
Lesson 13
Why do antibiotics sometimes not work?
A population of bacteria is made up of individuals
It is important to remember that when we consider a growing population of bacteria within an infected person, it is composed of individuals. Those individuals may have small differences in traits, and may move around to different parts of the body. When we use antibiotics, the overall outcome is the result of drug molecules interacting with many, many individual cells.
Some bacteria avoid antibiotics
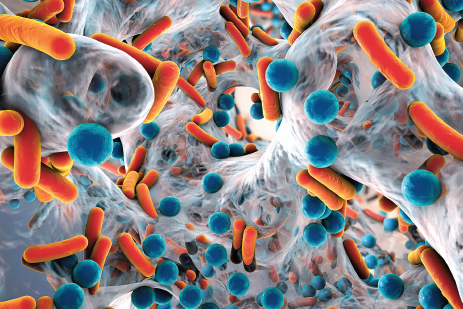
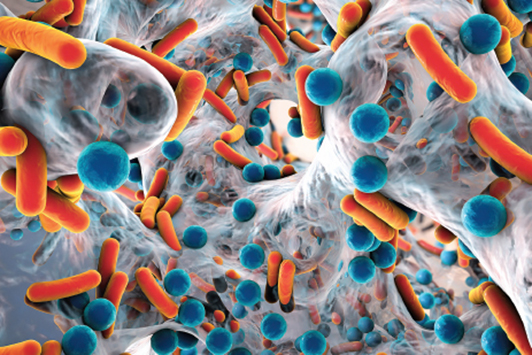
Sometimes bacteria infect an area that is relatively far from the bloodstream. In this case, the antibiotic may not reach the infected area in high enough amounts to kill or stop the growth of the bacteria. Other bacteria cluster together and produce a variety of molecules and structures, forming an organized community group that protects the bacteria. This bacteria-containing matrix is called a biofilm. The biofilm traps nutrients and water that help the bacteria survive. It keeps antibiotics in the bloodstream away from the bacteria.
Some bacteria are resistant to antibiotics
Some individual bacterial cells can survive and grow even in a liquid or agar medium that contains an antibiotic. In a culture like this, bacteria cannot avoid the antibiotic. These bacteria survive because differences in their heritable traits can sometimes be an advantage, helping them to avoid harm from antibiotics.
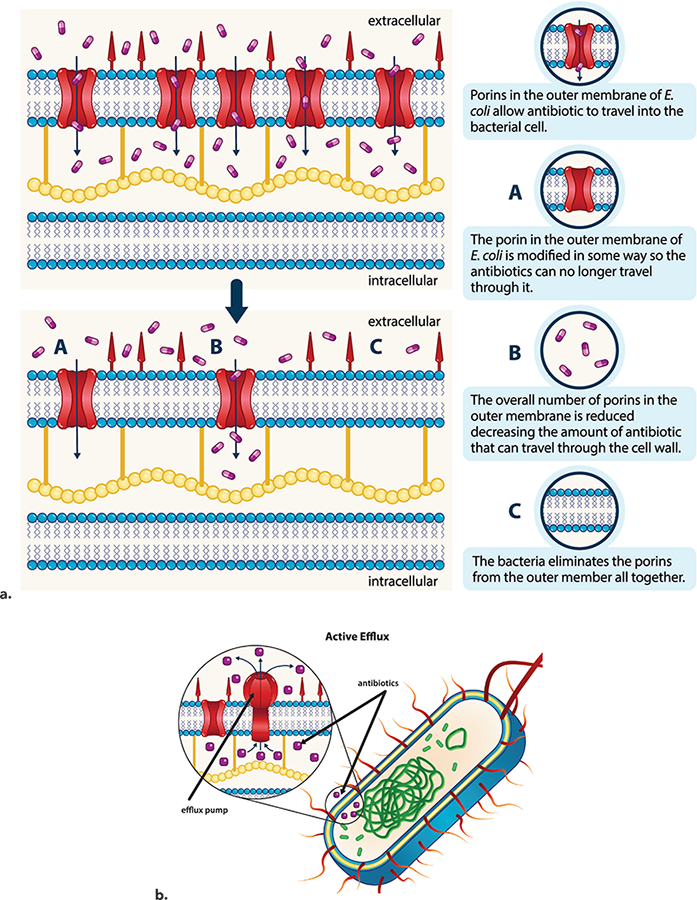
There are several different ways that an individual bacterium can be resistant to antibiotics. Some individuals have the trait of fewer porins, or holes through which substances can enter. This prevents an antibiotic from entering the cell in high amounts. Other individuals may have a trait for more molecular “pumps,” called efflux pumps, that can actually pump antibiotics back out of the cell after they enter it.
Two ways that bacteria resist antibiotics. a. Antibiotics cross bacterial cell membranes through proteins called porins. Resistant bacteria may have fewer porins, making it harder for antibiotics to enter. b. Some resistant bacteria are able to pump antibiotics out when they enter the cell.
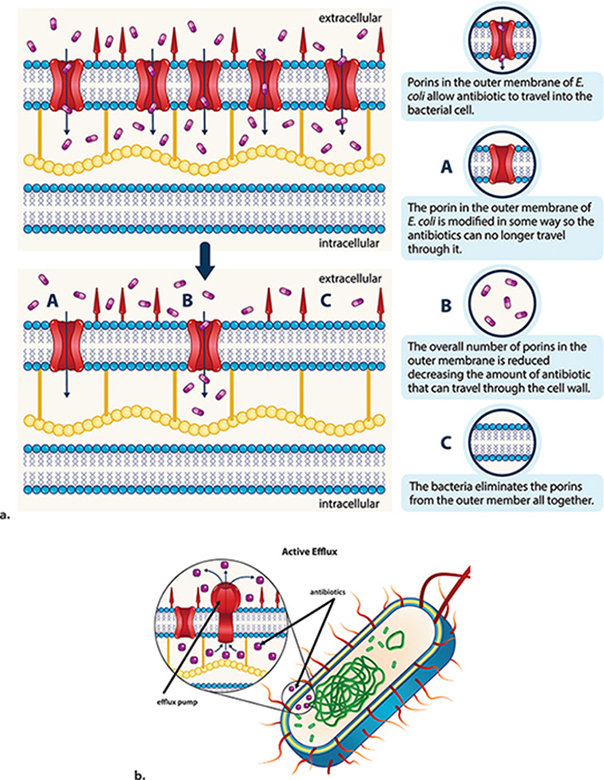
An individual bacterium with one or more of these helpful traits may be said to be antibiotic-resistant. Others, without these traits, may be referred to as antibiotic-susceptible.
What can medical professionals do about antibiotic-resistant bacteria?
Sometimes antibiotic resistance is only partial. In these cases, increasing the antibiotic dose may be an effective way to kill all or most of the bacteria. In other cases, doctors may have to use a different antibiotic to treat the infection.
Reference
Adapted in part from NIH Curriculum Supplement Series: Emerging and Re-emerging Infectious Diseases, BSCS, 2012, pp. 15–16.
Lesson 14
How do antibiotic-resistant bacteria become more common over time?
How do antibiotic-resistant bacteria arise?
When antibiotics were first used in the 1940s and 1950s, people began to think that bacterial diseases were a problem of the past. The antibiotics’ success was only temporary, however. By the 1980s, populations of disease-containing bacteria resistant to one or more antibiotics were common. Fortunately, newer and stronger antibiotics were still being discovered, so alternative treatments were available. But bacteria soon developed resistance to the new antibiotics, too. Today there are some populations of bacteria that are resistant to almost all of the antibiotics available to treat them.

How do entire populations of bacteria become resistant to antibiotics?
Imagine growing bacteria in liquid or agar medium. When you add an antibiotic to the medium, most of them are killed. But there may be one out of the million bacteria growing in the medium that happened to have a trait that made it resistant to the antibiotic. This bacterium survives and reproduces.
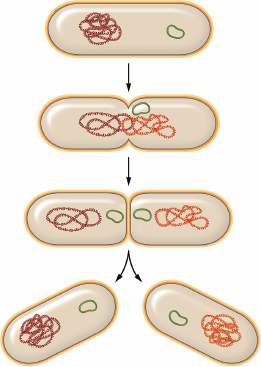
Asexual reproduction of bacteria. Bacteria grow to a certain size before they reproduce by making a copy of their DNA and splitting into two. Each new cell has an exact copy of the original cell’s DNA.
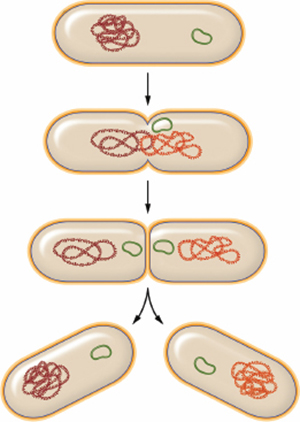
Bacteria reproduce asexually; that is, they do not need two parents to reproduce. Instead, individual cells grow to a certain point and then split more or less evenly to produce two cells, each having one copy of the DNA. The resulting two cells are identical to each other. This means that when an antibiotic-resistant bacterial cell in your medium reproduces, each of the new cells also has the advantageous trait. The new, resistant cells grow and reproduce, making more resistant bacterial cells. Meanwhile the susceptible cells are all dead. They do not add new cells to the population. The resistant bacteria survive and continue growing and reproducing without competition from the susceptible bacteria. Soon, all of the bacteria in the population are resistant to the antibiotic. This same process can take place inside the human body when antibiotics are used to treat an infection.
Natural selection explains how bacteria evolve to be antibiotic-resistant
The process just described illustrates the key observations that led Charles Darwin to the idea of natural selection. Darwin collected specimens and made observations of plants and animals around the world, including remains from extinct organisms. He used these observations to explain how populations could change over time.
Darwin’s observations |
Our example of antibiotic-resistance bacteria |
|---|---|
Individual organisms within a population vary from one another in particular traits. |
A few bacteria in the bacteriaI population had a trait that made them resistant to the antibiotic. |
Some variations among individuals can be passed from parents to offspring. |
When they reproduce, the resistant bacteria pass this gene for antibiotic resistance to the new cells. |
More offspring are born than can survive. |
Bacterial populations increase exponentially until they run out of nutrients and space.* |
Darwin’s conclusion |
Our conclusion |
Individuals that have inherited traits that help them survive and reproduce will leave more offspring. The frequency of these traits will increase in future generations. |
The antibiotic-resistant bacteria survive antibiotic treatment and reproduce more than the non-resistant bacteria. The percentage of resistant bacteria in the population increases over time. |
*We made this observation in chapter 1.
Comparison of natural selection to the case of antibiotic-resistant bacteria.
The basic idea of natural selection is that individuals who have traits that allow them to survive and reproduce more successfully in an environment will leave more offspring with those traits. The population will change over time as the environment “selects” the individuals that reproduce more successfully. Over the generations, the population will have more and more individuals who have those traits. In our example, the more we use antibiotics, the more the bacteria’s environment selects for resistant individuals. The antibiotics may eventually become ineffective for treating infections.