3.8 FDA Medication Safety Surveillance
Although every medication goes through a rigorous approval process, consumers should keep in mind that all drugs—prescription, OTC, and homeopathic, and all dietary supplements—have a risk of toxicity. In recognition of this fact, the FDA continues to gather information about any serious adverse reactions from approved medications. An adverse drug reaction (ADR) is defined as a negative consequence to a patient from taking a particular drug. Indeed, despite many years of research and clinical studies, some medications that enter the marketplace will still place individual patients at risk for a serious adverse reaction—an event that may not always be preventable or predictable. Even after millions of prescriptions are written (or vaccine doses administered) for patients of all ages, rare adverse effects may suddenly appear in the general population.
 Pharm Fact
Pharm Fact
Students may also hear the phrase ‘black box warning,’ which is another way to say boxed warning.
To protect the public’s safety, the FDA requires that drug manufacturers develop an information resource for pharmacy personnel, called the package insert (PI), including boxed warnings about any possibilities of an extreme ADR. Boxed warnings (which show up in patient, provider, and pharmacy personnel reference materials from the manufacturer, FDA, and drug reference collections) highlight dangerous side effects, interactions, and use of drugs. These boxed warnings must also be included in the patients’ information printout accompanying the medication. The FDA also established a nationwide surveillance system to serve as a conduit for reporting serious effects of certain medications. This Adverse Event Reporting System (AERS) is a centralized database that gathers and stores information from two separate programs: MedWatch for drugs and Vaccine Adverse Event Reporting System (VAERS) for vaccines. These will be covered in greater depth in Chapter 14 on safety. The FDA uses the collected information (with privacy protected) to track problems or issues that were not apparent when the medications and vaccinations were in clinical trials.
The recognition of a potential problem does not always mean that the product will be removed from the market. Many times, other initiatives are implemented to reduce or eliminate a safety risk—such as improving prescribing information, increasing awareness by educating healthcare professionals or the public, or perhaps simply changing the name of the drug or labeling. However, if significant incidents of ADRs come forth for any drug or vaccine, the FDA has the power to issue a drug recall (pull it off the market) with a marked level of urgency. Technicians and pharmacists must watch for these FDA recalls and immediately pull the products from their inventory, alerting patients when appropriate.
To avoid problems like those that occurred with thalidomide and other drugs, the FDA recognizes the need to do more prevention work with the high-risk drugs it has approved. It requires the manufacturers to develop Medication Guides, which provide patients with written consumer information on the high risks and proper uses of the drugs they have received. Medication Guides go beyond the usual patient instruction sheets.
However, some drugs require more detailed verbal and written communications and more focused patient monitoring. These drugs usually carry a high risk for serious adverse reactions if used inappropriately or by specific vulnerable populations. In these identified cases, the FDA requires that a risk evaluation and mitigation strategy (REMS) be developed by the drug manufacturers to ensure that the benefits of their drug outweigh the risks. For example, isotretinoin, a drug for severe acne, can cause serious birth defects if used inappropriately. Doctors and pharmacists must take special precautions to prevent pregnant or potentially pregnant women from using the drug.
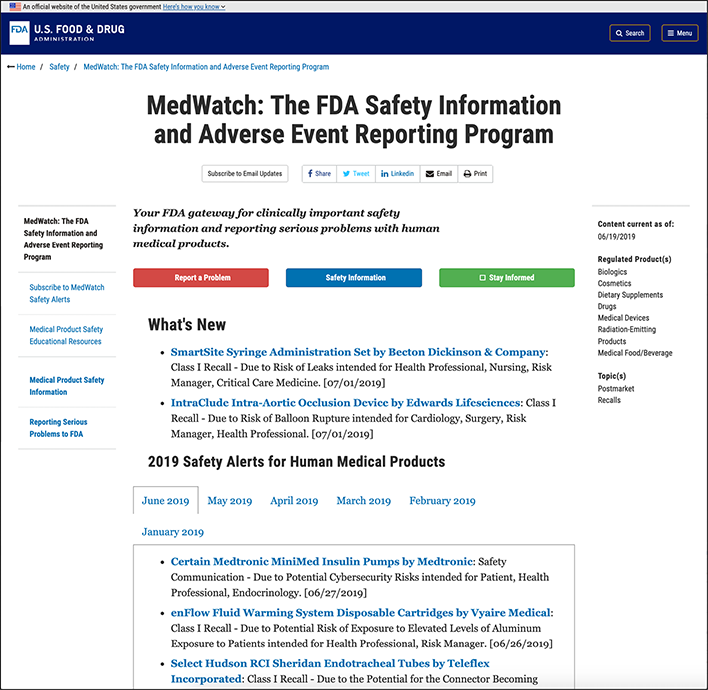
The FDA MedWatch website has the latest safety information on prescription drugs.
Drug manufacturers maintain a centralized database to monitor each patient more closely on these high-risk drugs and must make periodic assessment reports to the FDA on the status of the REMS for each drug. (Particular REMS will be discussed in Chapter 14.) Each prescriber and pharmacy must register with the pharmaceutical manufacturer and agree to the REMS policies and procedures before dispensing any of these drugs.