7.6 The Medication Reconciliation Process
After an initial review of the prescription and completing or updating the patient profile, the technician enters the new prescription into the profile via inputting or scanning. The correct entry of the prescription is so critical because many drugs have similar names, and the incorrect drug or dose can be easily chosen from the drop-down menus in the computer database.
 Work Wise
Work Wise
If prescription problems arise, the technician should ask the patient whether he or she prefers to wait for the prescription to be filled and, based on workload and staffing, provide a good estimate for the waiting time to allow the patient to elect to wait, shop, or run errands.
Also, any written comments by the prescriber must be included in the database and on the medication label. For example, a narcotic prescription may include “may cause sedation,” “do not fill until [date],” or “refill no sooner than every 30 days.” Likewise, a prescription for an antibiotic may include “take for 10 days” or “take with food.” All of these instructions must appear on the medication container label for the patient. Once the pharmacist has approved the profile and the entered prescription, the medication reconciliation process can begin.
The Drug Utilization Review
The first step is to run the drug utilization review (DUR), which scans the patient profile to identify any problematic interactions that could occur as a result of the new prescription. The pharmacy software will concurrently transmit the prescription online for insurance processing. When the DUR detects potential problematic reactions, it offers warning alerts and action steps. There are many reasons a new prescription may be problematic:
allergies (like a penicillin allergy)
a complicating medical condition (like diabetes or asthma)
duplicate of a similar drug already prescribed (for example, two different drugs or narcotics for migraine headaches)
it has been prescribed in doses too low subtherapeutic or too high (toxic) for the patient (as with pediatric or geriatric patients)
it may not be safe or should be used only with caution for the patient because of being part of a vulnerable patient population (for example, women of childbearing age or who are pregnant or breast-feeding)

While no one likes to wait, accurately and safely processing a prescription has to take priority over rushing to keep someone from waiting.
The DUR always offers an onscreen alert or alert code for any potential adverse drug reactions (ADRs), which are negative consequences from taking a particular drug or mix of drugs. The harmful responses can range from skin reactions and breathing problems to temporary injury, permanent disability, or death. An ADR can also create an allergy (hypersensitivity reaction) if that drug or a similar drug is taken again. Different pharmacy software programs, online networks, and insurance companies use different DUR codes, abbreviations, and messages, but all offer alerts (see Table 7.6).
Table 7.6 Sample of Drug Utilization Review Screen Codes
Administrative |
Dosing/Limits |
Drug Conflict |
Disease Management |
Precautionary |
|---|---|---|---|---|
AN – Prescription Authentication |
ER – Overuse |
AT – Additive Toxicity |
AD – Additional Drug Needed |
DF – Drug-Food Interaction |
CH – Call Help Desk |
EX – Excessive Quantity |
DA – Drug-Allergy |
AR – Adverse Drug Reaction |
DL – Drug-Lab Conflict |
MS – Missing Information/ |
MX – Excessive Duration |
DC – Drug-Disease (inferred) |
CS – Patient Complaint/ |
DS – Tobacco Use |
NA – Drug Not Available |
HD – High Dose |
DD – Drug-Drug Interaction |
DM – Apparent Drug Misuse |
OH – Alcohol Conflict |
NC – Non-Covered Drug Purchase |
LD – Low Dose |
DI – Drug Incompatibility |
ED – Patient Education/ |
SE – Side Effect |
NF – Non-Formulary Drug |
LR – Underuse |
IC – Iatrogenic Condition |
ND – New Disease/ |
|
NP – New Patient Processing |
MN – Insufficient Duration |
ID – Ingredient Duplication |
NN – Unnecessary Drug |
|
PS – Product Selection Opportunity |
NS – Insufficient Quantity |
MC – Drug-Disease (reported) |
PC – Patient Question/ |
|
P – Plan Protocol |
SF – Suboptimal Dosage Form |
NR – Lactation/ |
PN – Prescriber Consultation |
|
TP – Payer/ |
SR – Suboptimal Regimen |
PA – Drug-Age |
RF – Health Provider Referral |
|
|
|
PG – Drug- |
SD – Suboptimal Drug/ |
|
|
|
PR – Prior Adverse Reaction |
TN – Laboratory Test Needed |
|
|
|
SX – Drug-Sex |
|
|
|
|
TD – Therapeutic Duplication |
|
|
Once a DUR message appears, the technician must show it to the pharmacist, who will then guide and help the technician to review and resolve the problem. The technician also needs to explain to the patient that a potential medication problem exists that must be resolved prior to dispensing. For example, if hydrocodone, a codeine derivative, is prescribed to patients whose profile indicates that they are allergic to codeine, then a precautionary message or code, such as DA, meaning Drug Allergy, will pop up. The pharmacist will check the patient profile for prior use of the drug and/or ask patients whether they remember taking hydrocodone without an allergic reaction. Similarly, if a patient is allergic to penicillin, the computer will generate a red flag if cephalexin (Keflex), a related antibiotic, is prescribed.
 Safety Alert
Safety Alert
As a technician, never perform or acknowledge a DUR. Once it has been acknowledged, the system thinks that it has been addressed, and the pharmacist’s opportunity to decide a course of action or counsel the patient is lost. All software actions related to a DUR pertaining to drug interactions should be executed by a pharmacist for safety.
The technician cannot override DUR flags without pharmacist review, but the technician generally does prioritize the alerts for the pharmacist in terms of urgency. The DUR is an extremely important shared responsibility of the technician and the pharmacist. A missed drug allergy or serious drug interaction can cause great patient harm or even death and could also trigger a major negligence lawsuit.
The insurance response often comes back during the DUR. It provides additional alerts and action steps, some of which the technician can directly handle, such as notifying the patient that there is an “early refill” rejection. (Insurance processing will be covered in Chapter 8.) The technician, however, can notify the patient that there is an “early refill” rejection by the insurance provider.
 Safety Alert
Safety Alert
The technician must not rely just on the software but must also be on the lookout for any possible problems and let the pharmacist know.
The DUR and insurance processing steps are specifically designed to provide an additional level of protection to catch problems before they can occur. The processes address two real-world pharmacy practice issues: (1) no pharmacist (or prescriber) can remember all doses, adverse effects, and drug interactions for all medications, especially while juggling a typically busy medical office or pharmacy workload; and (2) a complete centralized medication profile usually does not exist, because patients often go to more than one pharmacy or more than one physician.
The pharmacy software catches issues from the patient profile, while the insurance software often catches problems with medications received at other pharmacies, among other issues. However, when a patient is taking unlisted OTC medications and supplements or using alcohol or other substances, it is not possible to assess the full potential of drug issues. That is why it is a “best practice” for the pharmacy technician to ask for additional information about these uses to enter them into the patient profile, or have the pharmacist discuss all of this with the patient in conversation or a medication therapy counseling appointment.
 Safety Alert
Safety Alert
Technicians and pharmacists have to fight alert fatigue, or getting so used to common alerts that they are not taken seriously. Some computer systems lock up after alerts until the pharmacist resolves the issues and unlocks the system.
Pharmacist Responses to Drug Utilization Review Alerts
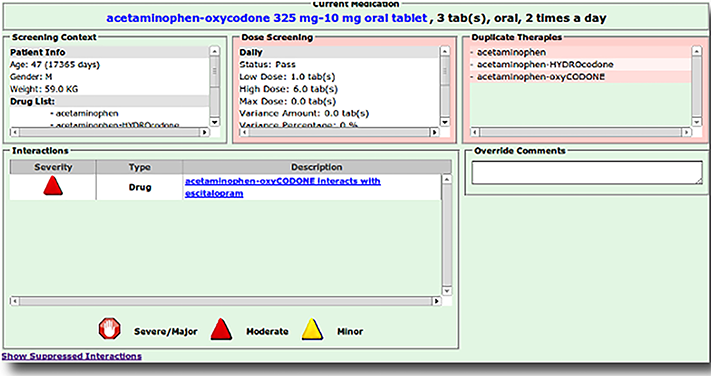
Most DUR notifications are categorized by their potential severity: mild, moderate, or severe (see Figure 7.9). Generally, the pharmacist must document the actions taken on moderate and severe alerts. Sometimes the needed response is listed on-screen. The pharmacist must use professional judgment to review the profile and assess the significance. Then the pharmacist must determine what type of action, if any, is necessary. Options include the following:
contacting the prescribing physician for more information or options
counseling the patient on potential issues prior to dispensing
overriding the DUR and filling the prescription
The pharmacy technician will not be able to proceed to fill the prescription for the patient until the pharmacist resolves the DUR alert(s). Often the pharmacist will write a reminder note that the patient needs counseling about the drug’s use and potential effects. When the patient arrives to pick up the medication, the technician will tell the pharmacist so that this conversation can happen.
Figure 7.9 Sample DUR Alert
When pharmacy software detects a potentially serious drug interaction, the technician must alert the pharmacist to have it resolved before filling and dispensing.