12.3 Hospital Infection Prevention
Infection control is the responsibility of all healthcare workers. It involves two aspects—stopping transmission of disease agents (prevention) and killing germs that exist on instruments and surfaces and in facilities (destruction). Healthcare facilities must continually do both.
Patients and employees are only safe from infectious processes when everyone working in the hospital follows good infection control techniques. Guidelines and recommendations to prevent infections are developed at the national, state, and facility level.
The Centers for Disease Control and Prevention
At the national level, the Centers for Disease Control and Prevention (CDC) set guidelines for hospitals and healthcare workers. State departments of health also set policies and procedures to prevent and address state public health issues and disease outbreaks. The CDC recommends that healthcare workers receive an annual flu shot (usually free of charge), and the CDC developed the universal precautions for preventing transmission of blood-borne infections for all healthcare workers who have any potential contact with any blood or bodily fluids (mucus, urine, semen, lymphatic fluid, excrement, and sebum). These precautions work to protect healthcare workers and patients from HIV, tuberculosis, hepatitis B and C, MRSA, and many other HAIs.
Generally, technicians in hospital pharmacies or sterile compounding facilities do not have potential contact with blood or other bodily fluids, but they need to be cautious to cover any open wound and follow the universal precautions and infection-control procedures of the department. Pharmacists who provide direct patient care and administer vaccines at healthcare fairs do encounter situations where they have potential contact; in these situations, they apply the prevention and disposal precautions shown in Table 12.1.
Table 12.1 Universal Precautions for Prevention of Blood-Borne Infection Transmission
|
 Name Exchange
Name Exchange
Another term for healthcare-associated infections (or healthcare acquired infections) is nosocomial. The Greek term nosokomos refers to someone who tends the sick, so a nosocomial infection comes from someone working to heal those who are ill.
The Infection Control Committee
Each hospital’s Infection Control Committee is responsible for following CDC guidelines by developing hospital-specific policies and procedures. The Infection Control Committee (ICC) is generally composed of physicians, nursing staff, infection control practitioners, quality assurance personnel, and risk management personnel, as well as representatives from microbiology, surgery, central sterilization, and environmental services. A pharmacist with an interest and expertise in antibiotics is also a member of the team. The goal of this interdisciplinary team is to bring together individuals with expertise in different areas of health care to oversee the infection control procedures and training of all healthcare workers, track hospital infection rates, monitor trends in antimicrobial medication use, and address any specific threats and ongoing problems.

The Infection Control Committee (ICC) develops procedures with the hospital to prevent or address HAI outbreaks as well as other infection-fighting issues.
The CDC recommends that the hospital’s ICC documents the incidence of HAIs and the use of antibiotics, and periodically checks to assess the adherence of staff members to hand-hygiene guidelines. The committee is also responsible for educating hospital personnel on the importance of receiving all necessary vaccines. Lastly, the committee plays a major role in ensuring that the hospital maintains compliance with the Joint Commission accreditation standards regarding all infection control procedures.
Tracking and Addressing Healthcare-Associated Infections
To reduce the possibilities of occurrences of HAIs, also known as “nosocomial infections,” the ICC works to identify and fix any gaps or problems in procedures or training. When outbreaks occur, the committee is responsible for investigating to determine the infective source(s). It then recommends implementation of changes in protocols and new education measures and materials to correct the deficiency. For instance, the committee may evaluate whether new sanitizing chemicals or sterilization processes should be used in the surgical operating rooms. If resistance of particular microorganisms to a specific antibiotic is increasing, then the committee may review whether the antibiotic is being ordered or administered inappropriately. The hospital ICC might also recommend that all employees are properly vaccinated and that certain healthcare workers receive TB skin tests to ensure that they have not contracted the disease or are not carriers.
 Pharm Fact
Pharm Fact
Severe adverse effects from vaccines are rare (less than 1 in 100,000 administrations, according to the CDC)
Implementing Healthcare Worker Vaccinations
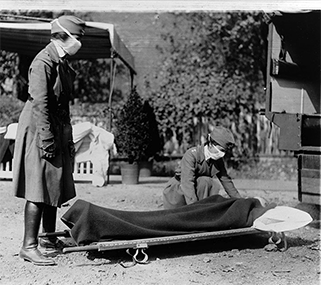
In St. Louis in October 1918, members of the Red Cross Motor Corps, all wearing masks against the further spread of the Spanish influenza epidemic, carry a patient on a stretcher into their ambulance. Spurred to prevent a recurrence of the devastation of the 1918 flu pandemic, scientists work on annual flu vaccines.
The most common vaccines recommended in the hospital are the annual flu vaccine and, for specific personnel, a series of vaccines against hepatitis B given over a six-month period. The hepatitis B virus is transmitted by exposure to blood and body fluids; it can cause acute and chronic infections of the liver.
The best time to get a flu vaccination is in September or October each year in North America because the immune system can take a few weeks to respond fully to the vaccine before the usual winter flu season starts. The benefits to the healthcare workers are that the flu shot usually keeps those individuals, their family members, and hospitalized patients safe from the flu strain that it was formulated to address, reducing the number of sick days.
Many individuals, especially those who are young and healthy, feel as though a flu shot is unnecessary; yet research has shown that the flu virus can be carried by asymptomatic healthy individuals and passed on to hospital patients with whom they have contact. Since many of these patients, especially older adults and young infants, have compromised or weakened immune systems, exposure to the flu virus can be deadly.
 Pharm Fact
Pharm Fact
In most years, when the most circulating seasonal influenza viruses are similar to the one in the vaccine, the flu vaccine is 60% to 70% effective. It is not 100% effective because the most current injectable flu vaccine is developed based on last year’s virus (it takes a year for development).

Vaccine developers use chicken embryos. These embryos incubate a form of the virus that is processed into a vaccine. Because of the egg connection, those with egg allergies need to receive a different flu vaccination formulation.
There are a few restrictions for obtaining a flu vaccine. Personnel with minor illnesses, such as a cold, can be vaccinated, but those who have an acute feverish illness need to wait at least 24 hours after the fever has subsided before getting the vaccine. Women who are pregnant can be vaccinated but individuals who are hypersensitive to eggs should not receive the flu vaccine as the virus is incubated in eggs.
 Safety Alert
Safety Alert
All pharmacy personnel should receive an annual flu vaccine to protect both themselves and their patients and families from contracting this virus.
 IN THE REAL WORLD
IN THE REAL WORLD
The flu virus mutates or changes every year, and scientists never know how virulent or contagious it will be. Occasionally, a virulent pathogenic influenza virus appears like the 1918 flu. The 1918 Spanish flu pandemic killed far more people than World War I—675,000 US citizens and servicemen died, which was 10 times the number of US soldiers killed in the war. In case of any epidemic or pandemic flu outbreak, all healthcare workers need to be fully vaccinated to protect themselves and care for the sick.
Despite these compelling reasons, 2018 CDC studies showed that only 78% of all healthcare workers received an annual flu shot, leaving approximately one out of four healthcare workers (and their patients) vulnerable. In October 2018, the CDC reported that only 37.1% of people age 18 and older in the United States received a flu vaccine, leaving most persons without the protection afforded by flu vaccination.
Contrary to popular myth, individuals cannot get the flu from most vaccines because these inoculations generally contain an inactivated (killed) virus. There is, however, a live attenuated virus (a weakened form) present in the nasal flu vaccine marketed as FluMist. This product is indicated for healthy children and adults from ages 2 to 49 who do not want a shot. Pharmacy personnel should be aware that some studies report that the use of the intranasal antiviral drugs may not be as protective as the injectable vaccine. In fact, the CDC recommended against the use of FluMist vaccine for the 2016–2017 flu season. However, FluMist was included in the recommended vaccine list for the 2018–2019 season.
The Advisory Committee on Immunization Practices (ACIP) has expressed concern over the use of the live, attenuated nasal flu vaccine for healthcare workers who care for patients in protective environments, such as intensive care or cancer care units. However, no documented transmission of this vaccine to patients has been reported. Most healthcare facilities allow healthy personnel up to age 49 who work in any setting to use the nasal flu vaccine, except those who care for severely immunocompromised patients.