12.4 Sterilization to Eliminate Microorganisms
All areas of the hospital or healthcare facility, including the general pharmacy, are responsible for cleanliness and infection-control procedures. The hospital aims for clean and sterile tools and sterile or aseptic surfaces, equipment, and intravenous fluids and medications. Sterile is the absence of any microorganisms, while asepsis is the absence of any destructive or harmful pathogens.
Aseptic technique is the set of special procedures used to ensure that harmful germs are not passed on or introduced onto surfaces and equipment, into the air, or into the compounded drug preparations. A person can never be “sterile” or completely free of germs. In everyday life, we wash our hands before we eat and after using the bathroom, cover our mouths and noses when we cough or sneeze, and avoid eating from each other’s plates or drinking from others’ cups when anyone is sick. These are all examples of simple everyday acts of infection control. We clean wounds with disinfectants and antibiotics before putting on bandages. These acts are a mix of preventive, aseptic, and sterile practices.
In the hospital, these methods become stricter and part of everyday routine. For example, rigid aseptic procedures are followed in the surgical, special care, and sterile compounding areas, and hospital instruments are either disposable or sterilized. Sterilization is the process that destroys all microorganisms or eliminates the conditions they need to live on surfaces, in liquids, and in the air. When an object (such as a medical instrument) is sterilized, the microbial life forms present are destroyed.
Many types of sterilization exist—dry and moist heat, distillation, mechanical, chemical, and ultraviolet—and a mix of all of these techniques is used in large hospitals. In some large university hospitals, the hospital pharmacy runs the central supply department that provides sterile supplies and sterilizes the surgical instruments. Consequently, pharmacy technicians particularly have to be familiar with sterilization methods and their clinical applications.
Heat Sterilization
Using heat to kill microorganisms is a an effective, economical, and easily controlled method of sterilization. It comes in two forms: dry heat and moist heat sterilization.
Dry Heat Sterilization
A traditional method of sterilization by dry heat is baking, which destroys microorganisms at intense temperatures. The higher the temperature, the shorter the time. Dry heat radiates off an object or organism first before penetrating, so higher temperatures and longer times are necessary for dry heat sterilization than for moist heat sterilization (to be explained next). For sterilization, a dry temperature of at least 170°C (338°F) must be maintained for a sufficient time, such as nearly two hours. For instance, hospitals bake blankets this way to sterilize them. Obviously, higher temperatures can also destroy the integrity of the tool, substance, or vehicle holding the microorganisms if it burns, boils, or melts. Therefore, one has to choose the right temperature and process. Facilities often use flame incineration for the disposal of contaminated objects.

An autoclave generates heat and pressure to sterilize. Most known organisms are killed in about 15 minutes.
Moist Heat Sterilization
Another traditional method for killing microbes is the moist heat sterilization method of boiling or steaming. Boiling kills many parasites, bacteria, viruses, and fungi in about 10 minutes, but more time is required to kill other microorganisms, such as bacterial and fungal spores and hepatitis viruses. If a water supply is of questionable quality, it should be boiled for a half hour before drinking. Automatic dishwashers loosely borrow concepts of both moist and dry heat sterilization during their hot water and drying cycles.
To sterilize instruments, the hospital and compounding facility use an auto–clave, a device that generates steam heat and pressure simultaneously (as mentioned in Chapter 10). When moist heat of 121°C (270°F) under pressure of 15 psi (pounds per square inch) is applied to instruments, solutions, or powders, most known organisms—including spores and viruses—are killed in about 15 minutes. At home, pressure cookers use the concept of heat and pressure to cook (and sterilize) vegetables. Moist heat is usually able to permeate into the microorganisms’ cells. However, hospitals are using moist and dry heat sterilization less frequently due to space requirements, equipment expense, and personnel training issues.
Distillation—Heat with Condensation
When a liquid such as water is boiled to kill microorganisms, chemical contaminants like mercury, lead, or arsenic remain. However, if the water is boiled and the steam gas vapor is sent through tubes to condense into distilled water, the chemical contaminants are removed. That is why distilled water, which is water in its purest liquid form, is the water that is boiled once more (for a sufficient time to kill any microbes that traveled with the vapor) to be used in sterile compounding. Distillation is an important decontamination process for liquids that can be boiled without changing their desired qualities.
Mechanical Sterilization—Filtration
For liquids and gases that would be radically changed by distillation or heat sterilization, one can use the mechanical sterilization method of filtration, which is the funneling of a liquid or gas through a screen-like material with pores small enough to block microorganisms. This method is used for heat-sensitive materials such as a culture medium (needed for growing colonies of bacteria or other microorganisms), enzymes, vaccines, and antibiotic solutions. Filtration can also be used to sterilize drinking water.
Filter pore sizes must be 0.22 micrometer (or micron) for bacteria and 0.01 micrometer for viruses and some large proteins. (A micrometer is 0.001 mm, or a millionth of a meter—for perspective, there are 25,400 micrometers to an inch.) Pharmaceutical manufacturing plants use both of these filters; hospitals and infusion facilities for home healthcare commonly use the 0.22 micron filters. Inserting a micrometer in-line filter in the lines of IV administration sets has been shown to reduce the incidence of infusion-related inflammation of the veins, as will be explained later in the chapter.
Chemical Sterilization
On surfaces that cannot be heated, hospitals use chemical sterilization with chemical gases, sprays, liquids, or wipes. As explained in Chapter 3, the English surgeon Joseph Lister first applied this technique during surgeries in the 19th century using a mild carbolic acid solution to prevent infection. Some forms of chemical disinfecting are still used to prevent pre– and postoperative infections. Few chemicals produce complete sterility, but many reduce microbial numbers to safe levels. Any chemical applied to an object (or the body) for sterilization purposes is known as a disinfectant. Iodine, isopropyl alcohol (IPA), and chlorinated bleach are common topical or surface disinfectants. The disinfecting solution of choice to clean equipment in surgical and sterile compounding areas is sterile 70% IPA solution.

In hospitals, many different disinfecting agents are selected for use, depending on whether they are used to clean tools, injuries, or hands. Chlorhexidine gluconate is an antiseptic germicidal agent used for aseptic handwashing in sterile compounding.
Gas Chemical Sterilization
Gas sterilization uses chemicals in their gaseous, or vapor forms, for disinfecting. Gas sterilization requires special equipment and aeration after application. Sealed equipment can automatically spray the gas ethylene oxide to sterilize objects that are too difficult or large to wipe down or that could be destroyed by heat. Ethylene oxide is highly flammable and is used only in large institutions and manufacturing facilities that have adequate equipment and ventilation to handle the gas. Many prepackaged IV fluids, IV administration sets, and bandages are manufactured in facilities that apply this type of sterilization. Ethylene oxide leaves a slight, harmless residue that can be detected as an odor.
Ultraviolet Sterilization
Light is also used for sterilization. Light rays come in different lengths, intensities of energy, and colored hues, all of which are on a spectrum and some of which our eyes are not able to detect and distinguish. The smaller the wavelength of rays, the more radiation of energy there is. Ultraviolet light is on the shorter spectrum, and it is more dangerous because of this. That is why we wear sunscreen to protect our skin from the sun’s ultraviolet rays, which are damaging to skin cells.
Ultraviolet (UV) radiation is the focused energy of these UV rays. UV radiation is damaging to living organisms, causing deterioration of cellular processes. That is why people for centuries have hung out their laundry and diapers in the sun to disinfect them. UV radiation can be used to sterilize air, gases, and surfaces. However, UV radiation does not permeate deeply, so only those elements directly touched by the UV rays are actually sterilized. Also, UV radiation is harmful to human eyes and skin, which is why you must avoid direct contact with the UV sterilization processes. That is why UV lights are turned on to sterilize rooms in evenings or off hours when personnel are not present.
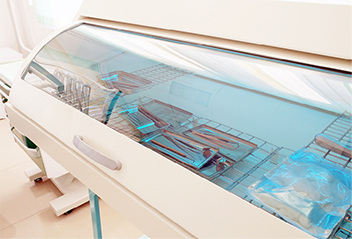
Sterilization boxes are used to sterilize surgical instruments.