13.3 Calculations
Though the label or Master Formulation Record may provide most or all of the calculations for compounding, there may be times when mathematics is required. Many pharmacy software programs automatically print the needed calculations for measurements and dosages of the drugs (the amounts needed to be drawn up or added) on the CSP labels.
 Safety Alert
Safety Alert
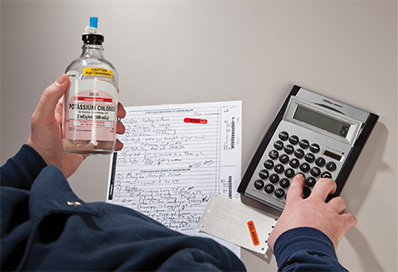
The IV technician is referring to a medication label to perform calculations.
However, inside the anteroom, the technician may need to compare the concentration of the dose ordered with the concentration of stock drug on hand and perform calculations to determine the desired volume of each ingredient to add to the LVP or SVP. The IV flow rates are also typically provided on the physician’s medication order. The technician then uses the ordered IV flow rate to calculate the days’ supply for IVs and IVPBs, and the pharmacist verifies the accuracy of the technician’s calculations as a double check. Hospital pharmacy technicians may also serve on cardiopulmonary resuscitation (CPR) or code teams that need to calculate dosages and drip rates for heart medications, prepare IV infusions and tubing, and attach IV sets.
For certain TPN preparations, neonatal (newborn) IVs, and chemotherapy IVs, the process is reversed. For these products, the pharmacist typically performs the first set of calculations, which are then verified by another pharmacist. The pharmacy technician then provides the “third-line check” of these calculations.
The IV technician must always double-check the medication order, labels, and calculations, documenting them all in the Compounding Record.
Common Compounding Calculations
As was demonstrated in Chapter 6 on calculations, numerous calculations may need to be done for different CSPs. The first calculations needed are often ones of measurement conversions, so it is essential to memorize the equivalents and metric conversions provided in Chapter 6. You will also need to know conversions from standard time (clock time) to military time since drug administration times in hospitals and other institutions are generally based on military time. Knowing how to translate temperatures in Fahrenheit to Celsius and back is essential for refrigerator and freezer storage conditions. (These conversions are also explained in Chapter 6.)

Checking and double-checking conversion measurements and IV calculations for children is especially important.
 Safety Alert
Safety Alert
Never rely solely on the directions on the CSP label or pharmacist’s calculations, or on your own. Always do the calculations and compare them to ensure accuracy.
Numerous other calculations are needed, and certain scenarios favor specific formulas and methods for the greatest accuracy. (But you will also have favored methods, based on what you know best.)
When a measurement is missing in an equation involving equal ratios, proportions, or fractions, the rate and proportion calculation method may be best.
For multi-stepped problems using conversions, dimensional analysis is usually favored.
For calculating concentrations based on the body surface area, use the proper equal ratios and proportion formula.
For addressing dilutions of powders and solutions, a combination of the ratio and proportion method and dimensional analysis can be used.
For mixing two different concentrations of the same drug, use the alligation method to find the amounts needed of each these solutions.
For working with milliequivalents for electrolytes and other solutes, there are specialized formulas.
 Safety Alert
Safety Alert
The metric system is typically used in the hospital setting. For this reason, all equations involving nonmetric measurements must be converted into metric (typically in the first step).
These are not the only calculations needed. In addition, one must know how to handle overfill concerns and calculate drip rates, drop rates, and infusion rates to determine 24-hour IV supply needs. Descriptions of these calculations are to follow.
Overfill Concerns in Admixtures and Dilutions
Although manufactured bags or bottles of medicated solutions are labeled to contain a set number of mL (e.g., 25, 50, 100, 250, 500, or 1,000 mL), the actual volume is greater because the containers include overfill. Overfill is the amount of solution that manufacturers add to make up for the loss of water due to evaporation through plastic. This loss is somewhat dependent on conditions during transport and storage and the ratio of fluid volume to the surface area. The larger the base solution of the IV bag, the greater the potential loss, so the more the manufacturers add overfill to compensate.
 Safety Alert
Safety Alert
Since there are often various ways to calculate the same answer, the best method to use is the one you are most comfortable with, using the information provided to you by the medication order, the CSP label, and the medication label.
Manufacturers are not consistent in their addition of overfill amounts, and they do not always label the overfill percentages they use. (See Table 13.8 for an example of overfill amounts.) Some overwrap their non-PVC (a type of plastic) IV solutions to reduce evaporation. These wraps should stay on until right before compounding or administration.
Table 13.8 Examples of Overfill in IV Bags
The amount of overfill varies with the manufacturer. |
Overfill Effects on IV Compounding Processes
There are four major ways to create admixtures for IV infusions, each affected by overfill rates to differing degrees:
Small-Volume Medication Addition for a Simple Admixture In this, you add the medication to the manufacturer’s base solution. But before doing so, you may need to reconstitute a powdered medication or dilute a concentrated medication by adding a diluent. These substances increase an IV’s volume. Generally, the SVP IV solution is meant to be infused to a patient until the bag is empty over a short period of time (such as 30 minutes)—as with antibiotics in an IV piggyback. In this situation, there is no need to compensate for overfill because the entire contents will be used and the full dosage will be received. However, the label should list the total amount of the drug and the total estimated amount of solution (including the estimated overfill). The label must also indicate that the CSP is meant for a single dose for a single short-term administration, and the IV tubing should be flushed to ensure that the whole dose is administered.
 Practice Tip
Practice Tip
IV solutions that are in non-PVC plastic may be more permeable to air and tend to evaporate, so manufacturers often place an outside wrap on them. You should leave the outer wrap on until going into the buffer room to discourage evaporation.
For example, you may receive a medication order for 20 mL of a drug solute in 100 mL of D5W to be administered over 30 minutes. To prepare the drug, you must add the 20 mL. The estimated overfill of the base solution bag is 7 mL, so the total volume in the SVP is equal to 127 mL. The IV label must read “Infuse entire contents for full dose.”
Volume Withdrawal and Medication Addition Another process is used when adding a large amount of medication to an LVP that is meant to be continuously administered until another IV filled with the same drug follows. Before adding the medication to the IV, a similar volume to that of the drug additive has to be removed first. For example, if you need to add 150 mL of a drug to 1,000 mL of a D5W solution, you must first withdraw 150 mL of the base solution before adding the medication. As with a simple admixture, the label should indicate the total drug amount and the estimated total volume of the solution, which would be the original 1,000 mL plus the overfill of the original base solution.
 Safety Alert
Safety Alert
An epidural pain medication must always be exact, with no overfill, so the base solution and the medication must be drawn into new syringes and then injected into a sterile medication reservoir cassette.
Larger Volume Withdrawal and Medication Addition When a large volume of an intensely concentrated dose is required, such as with a cancer chemotherapy drug, you may need to remove both the volume (diluent) of the medication to be added plus the estimated amount of the manufacturer’s overfill. That way, when the medication is added to the solution that remains, it will hold the prescribed dosage with no extra overfill solution to dilute it. However, if the overfill amount is not known but is just estimated, then it will still not be a precise dosage. Yet it will be far closer than if the overfill amount was never estimated for some accommodation of the volume. (See overfill calculation Example 1.)
 Safety Alert
Safety Alert
The only sure way to know a dosage is if the mixture is compounding into a new sterile container, and the label accurately indicates the percentage of drug solute to solvent, with no overfill to address.
New Container with Solute and Solvent For medications that need to be the most precise, as in chemotherapy, sterile compounding technicians need to work with accurate medication amounts and add them as well as the diluents and base solvent into a new sterile container. This can be done manually or in an automated compounding machine (as with TPN solutions). Using a new container means that there will be no overfill to calculate or estimate.
Overfill Policies
Each hospital and home infusion pharmacy will have written protocols for dealing with overfill calculations when using base solutions that have overfill. Small and large parenteral solutions are the majority of sterile compounded solutions, and normally the overfill amount does not appreciably affect the amount of IV fluids or drug dosages administered. In the case of IV neonatal drugs or cancer chemotherapy drugs that come in premixed solutions that must be reconstituted with a diluent before being transferred into a small or large volume parenteral solution, the combination of the overfill in the IV bag plus the diluent can cause an overdilution of the prescribed dose, especially if the entire contents of the IV solution are not administered. A diluted or less than prescribed dose of a critical drug may adversely affect the disease outcome.
 Practice Tip
Practice Tip
At the time of compounding sterile preparation, the volume of the actual overfill in manufactured products can only be estimated even if labeled because it is impossible to know how much solution has evaporated by the time of use.
Many pharmacies implement a 10% overfill rule for most medications where overfill issues are encountered. If the total calculated final volume to be administered equals 10% or less additional fluid, it is not necessary to withdraw any of the base solution.
For example, a medication order is received for a doxorubicin 90 mg solution to be added to a 1,000 mL (1 L) NS, with the compounded IV to be infused over six hours. Doxorubicin is available as a 2 mg/mL solution concentration; therefore, a 90 mg dose requires 45 mL of doxorubicin solution to be used.
If the manufacturer offers IV products with overfill amounts like those in Table 13.8, one liter of NS will contain approximately 50 mL of overfill. So 1,000 mL + 45 mL (of the diluent) + 50 mL (of overfill) = 1,095 mL. Ten percent of 1,000 is 100, so an overfill of an additional 10% would total 1,100 mL. Because 1,095 is under the limit of 10% more, no adjustment in the volume of the base solution (NS) would be needed, according to the 10% rule of hospital policy.
When the total calculated final volume to be administered equals more than an additional 10%, it is necessary to withdraw a volume of the base solution equal to the overfill volume plus the diluent of the drug.
Using the same example, if the 90 mg solution (45 mL) was to be added to 500 mL NS instead of 1,000 mL NS, then the final volume would have been 500 mL + 45 mL (volume of doxorubicin) + 30 mL (overfill) for a total of 575 mL. Since this volume is greater than the limit of 10% more of 500 mL (550 mL), the protocol states that 75 mL (45 mL + 30 mL) NS should be withdrawn before adding the medication solution of 90 mg, and 45 mL results in a final (and labeled) concentration of 90 mg of doxorubicin in 500 mL NS.
Example 1
A medication order says: Mitomycin 40 mg (0.5 mg/1 mL sterile water dilution), added to 1000 mL NS, infused over 6 hours. If the institution utilizes the 10% overfill rule, will this CSP result in an overfill that needs an adjustment of the base solution? Assume that the manufacturer uses overfill according to Table 13.8.
Step 1 |
Mitomycin 40 mg is available as a dry powder that recommends a concentration of 0.5 mg/mL. The amount of sterile water diluent to be added must be determined. First, convert from a decimal: Next, use the ratio and proportion method to calculate the volume of mitomyin required for a 40 mg dose. |
Step 2 |
One liter (1,000 mL) of NS will contain approximately 50 mL NS of overfill if the manufacturer’s proportion of overfill is similar to Table 13.8. Estimate the amount of overfill plus diluent. The final volume of the IV solution is equal to 1,130 mL, which is more than 10% of a liter (or 1,100 mL). Therefore an adjustment in the volume of the base solution (NS) is needed. |
Step 3 |
The hospital protocol states then that 130 mL (the amount of the overfill plus diluent) should be withdrawn from the 1,000 mL NS IV bag before injecting the medicated solution. |
 IN THE REAL WORLD
IN THE REAL WORLD
In August 2013, it came to light that more than 1,000 patients in some Ontario and New Brunswick hospitals received less than their required doses of their chemotherapy drugs because of confusion over the IV admixtures of cyclophosphamide and gemcitabine supplied by the compounding pharmacy. The problematic understanding arose between what the supplier contract requested and what was delivered, a problem increased by poor product labeling. The hospital pharmacy compounding personnel thought that the supplied IVs were concentrated forms of a multi-dose medication that required dilution while the manufacturer was providing single doses with overfill.
Because of this error, the cancer patients who received the compounded multi-doses were estimated to have received doses diluted between 3% and 20% from their medication orders. Family members of those who died of cancer may wonder whether their loved ones would still be alive if they had received their full-strength, medically ordered doses of the chemotherapy drugs.
Determining the Days’ Supply with IV Administration Flow Rates
To determine the correct number of IV bags needed for a 24-hour period and the time when a new IV bag will be needed, technicians at times must calculate the IV administration flow rates based on the size of the IV tubing and on the prescribed infusion rates. These calculations typically address the following questions that affect each other:
What is the infusion rate in mL/hour?
What is the size of the tubing and the drip rate (in gtts/min)?
How long will this bag last?
How much fluid has the patient received?
What time will the next bag be needed?
How many bags will be needed for the patient in a 24-hour period?
To answer these questions, you need to know the total volume of the ordered parenteral solution and either the prescribed infusion rate in milliliters per hour (mL/hr) or the number of hours over which the solution is to be infused. This information can be found in the physician’s medication order or in the Master Formulation Record directions. You then perform a series of IV flow rate calculations using either multiplication or division.
In the most simple sense, the infusion rate (R) is the volume divided by the time it takes (Volume/Time), and the time can be expressed in hours or minutes (and seconds if desired). The volume is expressed in mL.
To answer the question, “What is the infusion rate in mL/hr?” you must divide the IV volume in mL by the number of hours (hr) over which the CSP is to be administered (see Example 2, which follows):
To answer the question, “How long will this IV bag last (or take to administer)?” you must divide the total mL by the infusion rate (mL/hr) to determine the hours per IV bag (see Example 3):
or z; z is how long until 1 bag is empty
To answer the question, “What time will the next bag be needed?” you must add this length of time in hours (z) to the standard military time of the last administration of the infusion (see Example 4).
To answer the question, “How many bags will be needed for the patient in a 24-hour period?” you must divide 24 (the number of hours till resupply) by the number of hours calculated (z) that each bag will take to be infused (see Example 5). It is important to practice calculating examples of each equation.
Example 2
A physician orders
 4,000 mL of D5NS to be administered over 24 hours
4,000 mL of D5NS to be administered over 24 hours
What is the infusion rate in milliliters per hour?
Step 1 |
Begin by identifying the numbers to insert into the equation. Volume/Time = Rate , rounded to 167 mL/hr The answer rounded up is the infusion rate: 167 mL/hr. |
Step 2 |
Any hourly infusion rate can be converted into milliliters per minute by multiplying the answer by the conversion rate of 1 hour to 60 minutes. |
rounded to 2.8 mL/min |
|
Example 3
A physician orders
 500 mg of cefazolin in 50 mL of D5W to be administered as a secondary IV at 100 mL/hr
500 mg of cefazolin in 50 mL of D5W to be administered as a secondary IV at 100 mL/hr
How long will it take to administer this medication, or how long will it last?
z = 1/2 hour. The IV bag will take a half hour or 30 minutes to administer.
Example 4
A physician orders
 20 mEq of medication in 1,000 mL of D5W to be administered at 125 mL/hr
20 mEq of medication in 1,000 mL of D5W to be administered at 125 mL/hr
If the first bag is hung at 10:00 a.m., when will the next bag be needed?
Step 1 |
Apply the formula: or One 1,000 mL bag will last 8 hours. |
Step 2 |
Add the 8 hours to the last administration time of 10 a.m. |
So 1000 military time plus 8 hours equals 1800 military time or 6 p.m.
Example 5
A 1-liter LVP is running at 150 mL/hr. How many IV bags will be needed in a 24-hour period?
Step 1 |
Begin by converting 1 L to 1,000 mL, and then identifying the amounts to insert into the equation: per bag |
Step 2 |
Divide the 24 hours of the day’s supply by the hours per bag: bags for a 24-hour period So 3.6 bags will be needed, rounded to 4 full bags for a day’s supply. |
 Practice Tip
Practice Tip
If a calculation yields that a number of bags expressed by a decimal are needed, then an additional full bag is made. Fractional bags are never made.
Calculating Infusion Rates in Drops per mL and Drops per Minute
Sometimes it is important to know an even more precise calculation than the infusion rate to figure out how much medication a patient is receiving per drop and per minute. As described in an earlier chapter, the types of IV tubing selected have an influence on the infusion rates because they have a different drop factor, or drops per milliliter.
Macrodrip IV tubing may deliver either 10, 15, or 20 drops per milliliter. (Macro tubing comes in different diameters from manufacturers, resulting in some variance in drop factors.) In contrast, microdrip IV tubing delivers 60 drops per milliliter, so the drops are far smaller than the ones with macrodrip tubing. Macro tubing is generally used when more than 50 mL per hour needs to be administered, while micro tubing is used when fewer milliliters per hour are needed, such as in intensive care, pediatrics, or neonatology, when counting drops is important.
Most simple IV sets, if hung properly, use gravity to force the solution through the IV set to the patient, much as a water tower works to deliver tap water to city residents. However, many hospitals use an IV infusion pump or controller, which automatically adjusts the volume and administration rate of the infusion to fit the desired rate. The infusion pump is often integrated into the electronic medical record (EMR) and bar code point-of-care (BPOC) technologies to improve the accuracy of the IV administration and reduce medication errors.
 Put Down Roots
Put Down Roots
The Latin word for “drops” is guttae, which is then abbreviated as gtts.
Nursing personnel simply program the prescribed rate into the electronic infusion pump at the patient’s bedside. The rate can be digitally adjusted, causing the pump’s internal clamp to slow or quicken the rate at which the fluid flows through tubing routed through a chamber in the pump. Pumps can be set to give IV fluids in milliliters per hour or drops per minute.
To determine the rate in drops per minute, when the total volume and infusion time are known, the following formula is used (see Example 6):
 Practice Tip
Practice Tip
Always round down drips and minutes in drip rate solutions, especially for pediatric and neonatal patients.
Dimensional analysis may also be used to solve this type of equation. Since you cannot administer partial drops, it is common practice to round down answers with partial drops or minutes. For example, if the calculated answer is 20.6 gtts/min, it would typically be rounded down to 20 gtts/min.

An example of an IV set integrated with an infusion pump and bar code software records is the B. Braun Synchronized Intelligence Infusion Platform.
Example 6
An IV solution has a total volume of 250 mL and is being administered over 60 minutes using macrodrip tubing with a drop factor of 15 gtts/mL. What is the rate in drops per minute?
Step 1 |
Recall the drip rate formula previously given. Identify the values to insert into the drip rate formula. volume = 250 mL time = 60 min drop factor = 15 gtts/mL |
Step 2 |
Insert the values into the drip rate formula. |
Step 3 |
Round down the answer to 62 gtts/min. |
Example 7
An IV of D5W with 20,000 units of heparin is being administered at a rate of 40 mL/hr using macrodrip tubing with a drop factor of 20 gtts/mL. How many drops per minute is that?
Step 1 |
Use the drip rate formula previously given. Begin by identifying the amounts to insert into the formula. IV flow rate = 40 mL/hr drop factor = 20 gtts/mL |
Step 2 |
Insert the values from the problem statement into the formula to determine the drops per minute rate. First convert 1 hour to 60 minutes. The rate is 13 drops per minute (as rounded down to the nearest whole number). |
This problem can also be solved using the following dimensional analysis:
, rounded down to 13 gtt/min
Drop Rate Calculations for Medication Infusion Amounts Occasionally, pharmacy personnel can use drop factor calculations to determine the precise amount of a drug that will be infused per minute. These types of problems are sometimes referred to as IV drip rate calculations and can be solved by using dimensional analysis.
 Practice Tip
Practice Tip
To set up a problem logically, first identify the type of units needed for the final answer. Then list all the pertinent information, especially conversion rates, and their units. You can keep canceling out unneeded units, circling the ones that are needed.
Example 8
The prescriber has ordered a dopamine drip of an IV 800 mg in 250 mL of D5W. The IV will be administered at 10 mL/hr through microdrip tubing with a drop factor of 60 gtts/mL. How many milligrams of dopamine are in each drop? How many milligrams are received by the patient each minute?
Step 1 |
First determine the mg of dopamine per drop of the infusion using dimensional analysis. The patient will receive 0.053 mg of dopamine per drop. |
Step 2 |
Now calculate the mg of dopamine per minute of the infusion using dimensional analysis. The patient will receive 0.53 mg of dopamine per minute. |